The Circle of Willes in Cryonics Perfusion
Blood flows into the brain primarily via the carotid arteries and the vertebral arteries. The Circle of Willis is a circular arterial structure in the brain that connects blood flowing in from the carotid arteries with blood flowing in from the basilar artery (which is fed by the vertebral arteries).
Blood flows from the Circle of Willis into brain tissue via the anterior, middle, and posterior cerebral arteries. Many studies have shown that the Circle of Willis is incomplete in most people. A 1998 study of 150 healthy adult volunteers showed a complete Circle of Willis in only 42% of cases — more often complete in younger persons and females [RADIOLOGY; Krabbe-Hartkamp,MJ; 207(1):103-111 (1998)]. A slightly more encouraging 2002 study of 118 healthy volunteers in the 65-68 age group, showed 47% had a complete Circle of Willis [THE JOURNAL OF CARDIOVASCULAR SURGERY; Macchi,C; 43(6):887-890 (2002)]
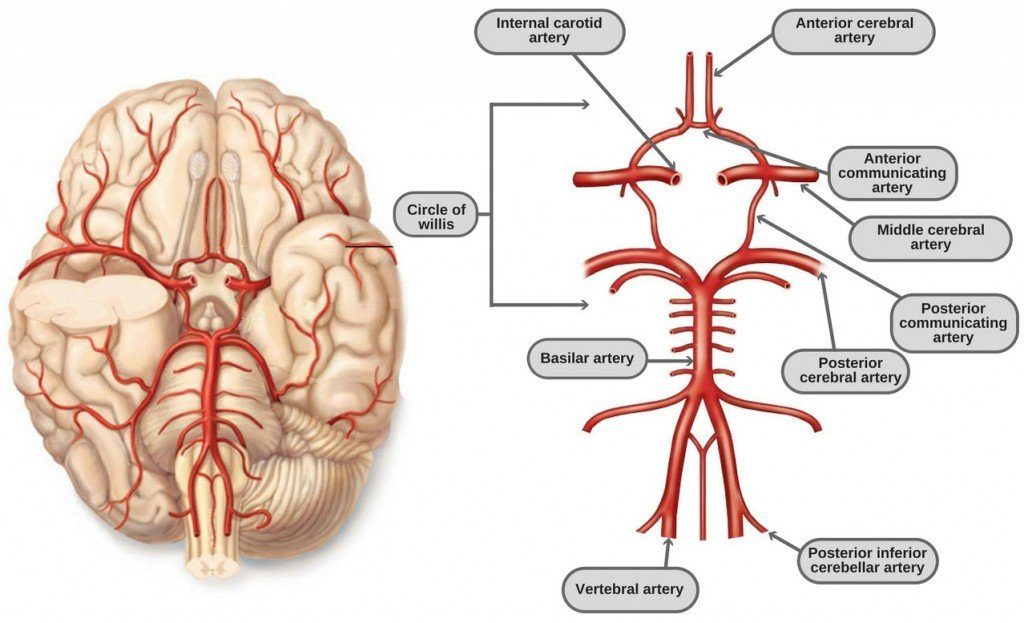
For cryonics purposes, it has been believed that perfusion into the carotid arteries, but not into the vertebral arteries will result in incomplete perfusion of the brain if the Circle of Willis is not complete. In particular, if both posterior communicating arteries are missing, then perfusing only through the carotid arteries will result in no blood getting to parts of the brain supplied by the posterior cerebral arteries. Both posterior communicating arteries were missing in 11% of those in the 1998 study and in 14% of those in the 2002 study cited above.
Nonetheless, a 2008 study showing Circle of Willis complete in only 40% of 99 patients found no case of insufficient perfusion in functional tests of patients given unilateral cerebral perfusion. The authors concluded that “extracranial collateral circulation” provides an alternative pathway to the Circle of Willis for cerebral crossperfusion [EUROPEAN JOURNAL OF CARDIOTHORACIC SURGERY; Urbanski,PP; 33(3):402-408 (2008)]. Although persons with missing posterior communicating arteries could easily have pathways to opposite sides of the brain, other variants of Circle of Willis incompleteness would be expected to prevent perfusion across hemispheres.
When the cryonics organization Alcor does a cephalic isolation (“neuro”) perfusion, the carotid arteries are initially cannulated and the vertebrals are not cannulated. Only when the patient is being perfused into the carotid arteries no flow is seen coming from the vertebral arteries are the vertebral arteries to be cannulated and the patient is to be perfused through both the carotids and the vertebrals. If, on the other hand, flow is seen coming from one of the vertebral arteries after perfusion of the carotids has begun, it is assumed that the Circle of Willis is complete and the vertebral arteries are clamped for the rest of the perfusion. Flow only needs to be seen in one of the vertebrals to confirm that the Circle of Willis is complete, because the vertebrals unite in the basilar artery before connecting to the Circle of Willis.
One Alcor employee has informed me that of 15-20 neuro patients perfused by this cephalic isolation method, not once has there been an absence of flow from the vertebrals and not once has Alcor perfused a cephalic isolation patient through the vertebral arteries. This would be slightly improbable, based on a 10-15% expected rate of incomplete communicating posterior arteries on both sides. But another Alcor employee remembers one or two cases where vertebral artery perfusion was done (which would match expectations).
When both posterior communicating arteries are not missing, there is another potential problem with perfusing only into the carotids and not the vertebrals — namely, loss of perfusion pressure. Perfusate entering the Circle of Willis could exit through the basilar artery (the vertebrals) instead
of through the cerebral arteries. Vascular resistance in the body is reportedly only one quarter what it is in the brain. Clamping the vertebral arteries (as is done during Alcor neuro perfusions) could prevent this problem. Blood flowing into the basilar artery need not be pushing all of the blood in the body, however, because arteries — and especially veins — have a large reserve capacity (a balloon-like ability to expand).
Possibly the reserve capacity of the brain would allow blood to flow into the brain as readily as into the body. Blood has about three times the viscosity of water, and vitrification solution has about twice the viscosity of blood. Viscosity will increase vascular resistance in all blood vessels, but the effect would be greater in the brain. The “no reflow” phenomenon would also create resistance in the blood vessels, which again might be greater in the brain than in the body.
Prior to the use of vitrification solution, the Cryonics Institute only perfused cryonics patients through the carotid arteries — there was no attempt to perfuse into the vertebral arteries. Nonetheless, dehydration was seen in the patients, and adequate effluent flow was seen from the jugular veins. Perfusion pressures were reportedly not excessive.
Currently, CI’s funeral director has been opening the chest (median sternotomy), and attempting to clamp the subclavian arteries, as well as the descending aorta, to perfuse into the ascending aorta. In several cases the ascending aorta has been perforated, forcing higher cannulations or the subclavians have been difficult to cannulate after having opened the chest. Our funeral director refused to open the chest at all for a known case of Methacillin- Resistant Staphylococcus Aureas (MRSA).
It would be preferable if a case could be made for perfusing all CI patients only through the carotids. Carotid-only has been recommended for vitrification perfusions overseas, as well as for glycerol perfusions in post-mortem sign-ups. Whether vitrification solution perfusion into the carotids can achieve adequate perfusion pressure in the brain — and whether adequate perfusion pressure can be verified by the observation of effluent from the jugular veins remains unresolved.
It should not be too difficult to clamp the vertebral arteries by cutting near the clavicle, as CI’s funeral director did when CI began the attempt to perfuse the vertebrals as well as the carotid arteries. Nonetheless, this would result in failure to perfuse portions of the brain supplied by the posterior cerebral arteries in the 10-15% of patients who are missing both posterior communicating arteries.
First published in The Immortalist, February, 2011