Medico-Legal Aspects of Human Cryopreservation Optimization
Introduction
Ongoing legal challenges and hostile interference of relatives have increased awareness among cryonicists that addressing the likelihood that one will be cryopreserved at all should take center stage among other strategies for survival. As a consequence, a number of individuals have recently taken on the task of working out the conceptual and legal challenges to minimize hostile interference (for a contribution on the ethical aspects of cryonics interference, look here).
One aspect of cryonics optimization planning that has received little attention to date is to develop legal strategies to deal with medical and legal issues surrounding one’s death, terminal illness, and the dying phase. In this memo I will outline some of the most important medical and medico-legal issues, how cryonicists could benefit from recognizing them, and suggest some legal and practical solutions. Before I get to the substance of these issues I would like to briefly identify all the stages in which proactive cryonics planning can improve our odds of personal survival.
Opportunities for cryonics optimization
The first and most obvious decision is to make cryonics arrangements. Alcor members face complicated decision making because the organization offers both whole body cryopreservation and neuro cryopreservation. From the perspective of cryonics optimization many members choose neuropreservation because it enables the organization to exclusively focus on what matters most; the brain. There is also a logistical advantage. In case transport of the whole body across state lines is delayed the isolated head can be released in advance as a tissue sample. Additionally, a number of Alcor members have recognized that it is possible to have the best of both worlds and combine neuro-vitrification and separate cryopreservation of the trunk. This allows the member to take advantage of the superior preservation of the brain that is available for neuro patients without having to forego whole body cryopreservation. This option is not widely advertised so one is encouraged to contact Alcor about revisions in funding and paperwork.
The other obvious decision is to have secure funding in place. Many members have given extensive thought about funding mechanism and wealth preservation so there is little need to discuss this here. From the perspective of cryonics optimization it is important to emphasize the importance of over-funding your cryopreservation. This not only protects you against future price increases, but also enables you to take advantage of technical upgrades that cannot be offered at the current preservation minimums. Another aspect to consider is leaving money to cryonics research. Although it is reasonable to expect that general progress in science will include general cell repair, there may be areas that will only be pursued by those who have a scientific or personal interest in resuscitation of cryonics patients. As in many areas in life, diversification is key. One should not solely depend upon Alcor or CI for successful resuscitation research or efforts.
Another important opportunity for cryonics optimization is to recognize the importance of proximity. From a technical point of view, there is simply no comparison to de-animating near the cryonics facility of your choice. This is not just a matter of reducing ischemic time. Remote standby and stabilization is a fertile ground for all kinds of logistical and legal complications. Most cryonics members do recognize the importance of reducing transport times but it is an established fact that as soon people become terminally ill they become more resistant to the idea of relocating and often prefer to die among friends at home. It is important to anticipate this scenario and to not delay relocation plans until the last minute. Another advantage of relocating at an earlier stage is that one is better protected in case of a terminal disease with rapid decline or sudden death.
As mentioned above, one issue that is getting increasing attention is how to protect oneself against hostile relatives and third parties. The take-home message is to alter cryopreservation contracts and your paperwork in such a matter that there is an incentive *not* to interfere.
Last but not least, something should be said about community building. Cryonicists can greatly benefit from becoming active in their local cryonics group. Often these meetings are open to members of all cryonics organizations. Most cryonics groups organize standby and stabilization trainings where members can familiarize themselves with the basics of the initial cryonics procedures. Such groups may not only play a part in your own future cryopreservation but are also useful to get a basic understanding about what you can do in the case a local member or a loved one needs to be cryopreserved. Another important aspect of participation in a local cryonics group is that one remains in contact with other cryonicists. When people get older their friends and family members die and the member has little communication with those who are aware of his desire to be cryopreserved. If you live in an area where there are no local cryonics groups contact your cryonics organization and/or start your own local group.
Physician-assisted dying
If there was more widespread acceptance of cryonics the harmful delay between pronouncement of legal death and the start of cryonics procedures would not exist. After a determination of terminal illness, preparations would be made to ensure a smooth transition between the terminal phase and long term care at cryogenic temperatures.
Some states have enacted legislation that allows a terminally ill patient to request the means to terminate their life. Assisted suicide is currently legal in the following three states: Oregon, Washington, and Montana. Physician-assisted dying does not remove the current obstacle that cryonics procedures can only be started after legal pronouncement of death but it can bring the timing of death (and thus of standby) under the patient’s control. Utilizing such laws can also greatly reduce the agonal phase of dying and its associated risk of damage to the brain.
The legal requirements for utilizing physician-assisted suicide can vary among states but, as a general rule, require that a patient has been diagnosed with a terminal illness with no more than six months to live, that the patient is of sound mind, and that the request is made in written form and witnessed. The State of Oregon has a residency requirement to discourage physician-assisted dying tourism.
Since cryonics procedures are performed after legal death, there is no reason why cryonics patients are exempt from utilizing these laws. Despite rumors to the contrary, there is no evidence that utilization of these laws require mandatory autopsy. After all, the cause of death in physician-assisted dying is clear; self- administration of the lethal drug. To avoid any possible accusations that cryonics organizations encourage the use of such laws, it is recommended that no person associated with the cryonics organization should be a witness, let alone be the physician that prescribes the lethal drugs.
Sudden death and autopsy
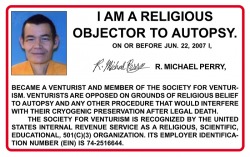
One of the worst things that can happen to a cryonics member is sudden death. Especially when the patient is young with no prior heart conditions, an autopsy is almost guaranteed. There is little one can do to avoid sudden death aside from choosing a lifestyle that reduces cardiovascular pathologies. The only preparation for dealing with sudden death is to become a religious objector to autopsy. Some states (including California, Maryland, New Jersey, New York and Ohio) have executed laws to restrict the power of the state to demand an autopsy. Although exceptions can still be made in cases of homicide or public health there is little to lose in using such provisions. The websites of Alcor and CI have links to the relevant forms to execute. The Venturists are offering a card for their members stating that they object to autopsy. This card can be requested from Michael Perry () at Alcor. An example of such a card is provided below.
Sudden cardiac death is not the only reason for ordering an autopsy. An autopsy is typically ordered if there are criminal suspicions (homicide) or suicide. There is also a greater risk of autopsy when a patient dies in absence of other people. Since many old cryonicists are single and spent a lot of time alone they are also at an increased risk for autopsy. This is another good argument to remain involved with local cryonics groups and in frequent contact with other cryonicists.
If autopsy cannot be avoided it is important that the cryonics organization is notified promptly. Cryonics organizations can make another attempt to persuade the authorities to abstain from an autopsy or to request a non-invasive autopsy that exempts and protects the brain. The cryonics organization can also issue instructions for how the patient should be maintained prior, during and after autopsy. It might be worthwhile to generate a template of general autopsy instructions for cryonics patients. Such a document may not be binding but it could be useful in limiting the amount of ischemia and injury.
The dying phase and Advance Directives
Most cryonics members have a basic understanding of the importance of time and temperature to protect a cryonics patient after legal pronouncement of death. Fewer people recognize the effect of the dying process itself on the outcome of a cryonics case. In best case scenarios (physician-assisted dying, withdrawal of ventilation) the dying phase is relatively rapid while in worst case scenarios extensive ischemic injury to the brain is possible. Little work has been done to outline recommendations for the terminally ill cryonics patient. One of the main objectives of this article is to recognize that cryonics members could benefit from a general template that can be used in their Advance Directives and to guide surrogate decision makers.
At this point it is useful to briefly describe how the dying phase itself can affect the outcome of cryonics procedures (for a more detailed treatment see the appendix at the end of this article). A useful distinction is that between terminal illness and the agonal period. A patient is classified as terminal when medical professionals establish that the patient cannot be treated with contemporary medical technologies. During this period the patient is usually still of sound mind and able to breathe and take fluids on his/her own. Unless the patient has suffered an insult to the brain or a brain tumor, there is no risk for ischemic injury to the brain yet. At some point, however, the body’s defense mechanisms will be overwhelmed by the patient’s disease and the patient enters the agonal phase. The agonal phase, or active dying phase, can be characterized as a form of general exhaustion. The body is still fighting but with decreasing success and efficiency. One of the biggest concerns for cryonics patients is the development of (focal) brain ischemia while the (core) body is still mounting its defense.
It would be impossible to design an Advance Directives template that is optimal for all cryonics patients, but there are a number of general guidelines that can inform such a document:
* All health care decisions should be guided by the objective of preserving the identity of the patient throughout the terminal and dying phase.
* Measures to prolong dying should only be initiated or accepted if they result in less ischemic injury to the brain.
* Life-sustaining measures should be withheld in case of traumatic or ischemic insults to the brain.
To ensure that sensible decisions are made in situations that are not covered by these Advance Directives, a Health Care Proxy can be executed that designates a person to make those decisions. It is understandable to give such power to the person closest to you but in the case of cryonics it is recommended that this responsibility should be given to a person with a strong commitment to your desires and a detailed understanding of the medical needs of cryonics patients.
Pre-medication of cryonics patients
If a critically ill cryonics member is at risk of ischemic brain injury during the dying phase it stands to reason that some palliative treatment options are better than others. One possibility for cryonics patients is to specify such options in one’s Advance Directives. Another scenario in which pre-medication is possible is where the medical surrogate is strongly supportive of such measures. It should be noted that such a decision rests solely with the member or his/her medical representative. Cryonics organizations should not be involved in the pre-mortem treatment of the patient.
There are two important questions about pre-medication of cryonics patients:
1. Is it safe?
2. Is it beneficial?
The answer to the first question has a lot to do with the status of the pharmaceutical agents in question. For example, a supplement like melatonin is less controversial than a prescription drug like heparin. The most important thing to keep in mind is that drugs that may be beneficial after legal pronouncement of death could have adverse effects in critically ill patients. Good examples are drugs that have effects on blood rheology and clotting. One would rather forego the hypothetical benefit of a drug if there is a non-trivial change of triggering major controversies about drugs taken during the dying phase. This leaves only certain supplements as relatively safe options for pre-medication of cryonics patients.
The answer to the second question is not clear. The rationale behind pre-medication is that it can protect the brain during agonal shock and its associated ischemic events. Evidence for this belief is usually found in the peer reviewed literature on neuroprotection in ischemia. However, there is a clear difference between the administration of neuroprotective agents during the dying phase and the administration of neuroprotective agents prior to artificially-induced acute ischemia. One perspective is that such agents are beneficial but only delay the ischemic phase of the dying period. In this case supplements have little neuroprotective effect. An alternative perspective is one where such supplements do not alter the agonal course as such but provide more robust protection after circulatory arrest. Obviously, this matter is not of concern to conventional medicine so there is little evidence to make rational decisions. In light of the previous discussion, the current (tentative) verdict should be that a case can be made for pre-administration of neuroprotective agents but that these agents should be confined to “safe” supplements like melatonin, Vitamin E and curcumin. Whether such a regime would be beneficial needs to be decided on a case by case basis and is, therefore, more in the domain of the Health Care Proxy than Advance Directives.
Do Not Resuscitate Orders
Do Not Resuscitate (DNR) orders present one of the most challenging issues for cryonics optimization. On the one hand, we would like to benefit from any attempt to resuscitate us in case of sudden cardiac arrest (or any other acute events that can lead to death). On the other hand, we would not like to be subject to endless rounds of futile resuscitation attempts that can damage the brain.
One would be inclined to think that resuscitation attempts should be made in case of sudden insults or during surgery but that no resuscitation attempts should be made during terminal illness. In reality things are not that simple. For example, resuscitation may be possible after 8 minutes of cardiac arrest but the patient can suffer severe brain damage as a consequence. Such a scenario can be minimized by executing a DNR at the cost of foregoing any resuscitation attempts at all. Would this outweigh the benefits of successful resuscitation attempts? It is hard to see how an objective answer to this question can be given without taking a specific person’s views on risk and treatment into account. One way to mitigate this dilemma is to make a distinction in your Advance Directives between pre-arrest emergencies (for example, resuscitation should be permitted in the case of labored breathing but presence of heart beat) and full arrest. An in-hospital situation where resuscitation of a critically ill patient would be helpful would be where it would allow a cryonics standby team to deploy at the bedside of the patient. As can be seen from these examples, good resuscitation instructions for cryonics patients require a lot of attention to context. Because confusion could arise whether Advance Directives would include pre-hospital emergency procedures it is recommended to execute an explicit document if you want these cases to be covered – such a document could be complemented by wearing a bracelet.
Creating a general template
This article has identified a number of important medico-legal issues that need to be addressed by cryonicists to optimize their cryopreservation. It has become clear that in the case of many topics we would all benefit from uniform and effective language. The next step is to translate the concerns discussed in this document in clear legal language so that templates can be offered to all members of cryonics organizations to draft their own Living Will and Advance Directives. One potential problem of such a general template is that it may not conform to state regulations and needs additional tweaking to make it valid in the state where the person lives.
——————————————————————————————–
Appendix : Neurological damage during the dying phase
Securing viability of the brain by contemporary criteria is the most important objective of cryonics standby and stabilization. Recognition of how pathological events in the central nervous system can defeat this objective is of great importance. As a general rule, the risk for increased brain damage is higher during slow dying. For example, when the ventilator is removed from the patient who is not able to breathe on his own the time between this action and circulatory arrest can be short. Conversely, when a patient is going through a prolonged terminal and agonal phase (regional) injury to the brain can occur while the body itself is still fighting for its survival.
The human brain has little storage of excess energy. As a result, hypoxia causes the brain to deplete its oxygen reserves within 30 seconds. The energy depletion that follows cerebral hypoxia during the dying phase has a number of distinct effects: 1) excitation or depression of certain processes in the brain, 2) alteration in the maintenance of structural integrity of tissues and cells, and 3) alteration of neuromediator synthesis and release. The depletion of oxygen leads to a switch from aerobic to anaerobic energy production. As a consequence, there is an increase in the metabolic end-products of glycolysis such as lactic acid which decreases pH in the brain. After 5 minutes no useful energy sources remain in the brain, which can explain why the limit for conventional resuscitation without neurological deficits is put at 5 minutes as well. Because the dying phase leads to progressively worse hypotension and hypoxia the metabolic state of the brain after the agonal phase is worse than if there would have been sudden cardiac arrest.
Light microscopic changes have been observed in brain cells after 5 minutes of ischemia. Prolonged hypotension, as can occur in the agonal patient, can lead to the appearance of “ghost cells” and disappearance of nerve cells. Such observations provide evidence that structural changes, including cell death, can occur prior to clinical death. Another manifestation of hypoxia (or hypotension) is the progressive development of cerebral edema. The resulting narrowing of vessels and decrease of intercellular space can, in turn, aggravate energy delivery to tissues. Of particular importance for cryonics stabilization procedures is the development of no-reflow which can prevent complete restoration of perfusion to parts of the brain during cardiopulmonary support. There is no consensus as to whether no-reflow can occur as a result of prolonged hypotension (as opposed to complete cessation of blood flow), but an extended dying phase can set the stage for cerebral perfusion impairment after circulatory arrest.
The central nervous system does not shut down at once. Throughout the terminal and agonal phase alternations in the brain progress from minor changes in awareness and perception to deep coma. As a general rule, more recent and complex functions of the brain disappear earlier than the most basic functions of the brain. The uneven brain response to hypoxia may reflect different energy requirements, biochemical and structural differences, and/or the activation of protective mechanisms to preserve the “core” functions of the brain. The CA1 region of the hippocampus has been demonstrated to be uniquely vulnerable to ischemia. This presents a problem for contemporary cryonics since the objective of human cryopreservation is to preserve identity-relevant information in the brain.
This article is a slightly revised version of a paper that was submitted for the 4th Asset Preservation Meeting near Gloucester, Massachusetts.